Stress fractures are a common injury among first-time marathoners, often caused by the repetitive impact of running long distances. These small cracks in the bones, typically found in the feet or lower legs, occur when the body is not given enough time to recover between runs. First-time marathoners are particularly susceptible due to a sudden increase in training intensity or from wearing inadequate footwear. Repetitive striking of the ground with each step, combined with poor running form or weak muscles, can lead to these microfractures. The primary cause of stress fractures is overuse, but factors like improper shoes, running on hard surfaces, or inadequate nutrition can contribute. Symptoms include localized pain, swelling, and tenderness that worsens with activity. Early intervention is key to preventing further injury. A podiatrist can diagnose the fractures, provide a treatment plan, and offer advice on proper footwear, running techniques, and rehabilitation exercises to prevent future issues. If you are a first-time marathoner experiencing pain, it is suggested that you schedule an appointment with a podiatrist.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact Jeffrey Parrett, DPM from Parrett Podiatry. Our doctor can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
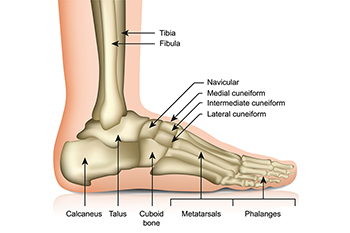
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
- Gender – They are more commonly found in women compared to men.
- Foot Problems – People with unusual arches in their feet are more likely to develop stress fractures.
- Certain Sports – Dancers, gymnasts, tennis players, runners, and basketball players are more likely to develop stress fractures.
- Lack of Nutrients – A lack of vitamin D and calcium may weaken the bones and make you more prone to stress fractures
- Weak Bones – Osteoporosis can weaken the bones therefore resulting in stress fractures
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact our office located in Waxahachie, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.